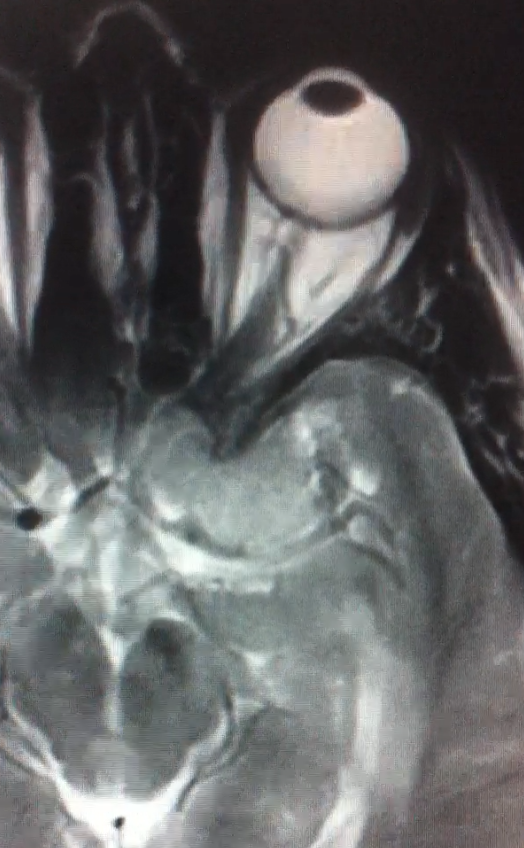
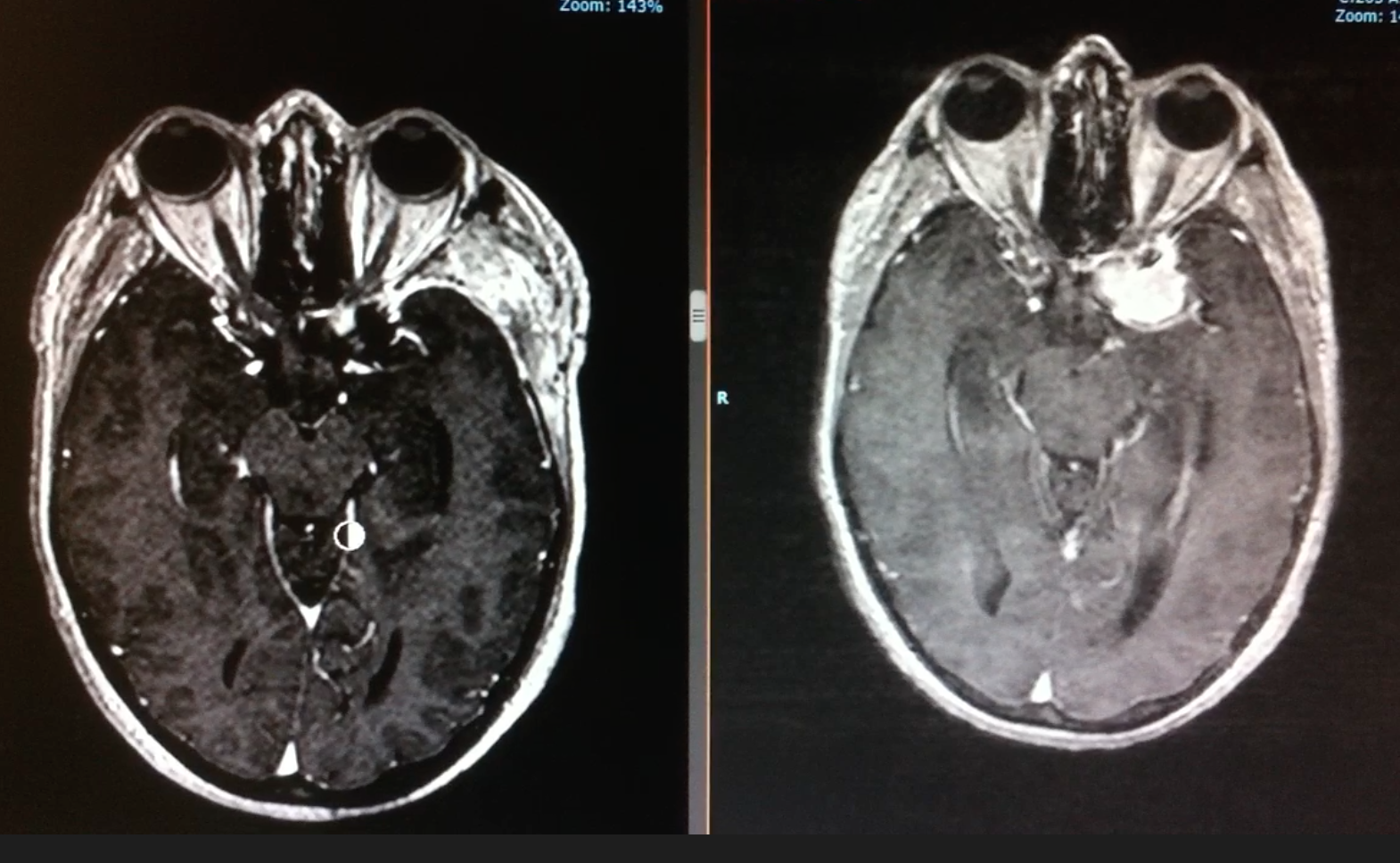
Left Clinoidal Meningioma
Published:
Left clinoidal meningioma diagnosed after epileptic seizure episode
HISTORY:
43 year old female who is brought to the emergency room after suffering an episode of epileptic seizures. Radiographic findings were consistent with a left clinoidal mass. The neurological exam was normal.
DIAGNOSTIC STUDY:
MRI brain showed left clinoidal extra-axial contrast enhancing mass compatible with a meningioma.
SURGICAL APPROACH:
Extended-pterional with extradural clinoidectomy
POSITIONING:
A Mayfield head clamp was applied. The patient was placed in supine position with the head slightly rotated (about 30 degrees) towards the right and extended such that the malar prominence would be the highest point in the surgical field. All pressure points were well-padded. The hair was clipped over the planned incision. Pre-prepping was done with chlorhexidine solution. The electrophysiology monitoring team inserted needles in their proper locations and baseline SSEPs, motor evoked potentials and, visual evoked potentials were obtained. The patient underwent co-registration of the preoperative stereotactic MRI with her surface landmarks.
OPERATIVE TECHNIQUE:
The area was prepped and draped in the standard sterile fashion. A fronto-pterional incision from the midline to the root of the zygoma, behind the hair line was planned and infiltrated with lidocaine and opened sharply using a #21 scalpel blade. Temporal muscle dissection was performed in two steps: interfascially below the frontal fat pad and then subperiostically to allow wider exposure and less tension on the muscle when reflecting throughout the operation.
Left pterioral craniotomy was performed using an electric high speed drill with the frontal cut extending to the superior orbital rim lateral to the supraorbital nerve. A burr-hole was placed at the anterior part of the frontospheoide suture (McCarthy) to expose both orbit and frontal dura. After careful dissection with a curved sharp dissector of the periorbit from the superior orbital wall, the orbital roof was cut with the aid of a 5mm chisel. The bone flap was uplifted in one piece (frontotemporal + supraorbital bar) utilizing a combination of #3 Penfield and Adson periosteal elevator with special care for the middle meningeal artery. The shenoid ridge was drilled down and waxed. The frontal sinus was not entered. The dura was noted to be intact. The bone dust was irrigated and suctioned clean.
The operating microscope was then draped and brought into the operative field. Careful dissection of the superior orbital fissure, elevating the osteal dura was performed with the aid of a Penfield dissector and gentle traction. The meningorbital band was cut with a #15 scalpel to expose the base of the clinoid process. The frontal dura was also elevated to reach the roof of the optic canal identifying its entry point. Under copious irrigation the optical nerve was unroofed using a diamond burr. Then the clinoid was hollowed progressively until the walls could be colapsed and movilized with a #6 Rhoton microdissector. Finally, the clinoid was removed and sent to pathology.
A C- shaped incision with base towards the sphenoid ridge was made and reflected. Microdissection began with a small anterior opening of the sylvian fissure with microscissors. After protecting the cortical surface with cottonoid patties the surface of the tumor was exposed. An initial biopsy was performed for pathological analysis and debulking began avoiding bipolar cautery. Sparing of arachnoidal plane was key for microdissection, that was performed bimanually with Gerald forceps and microscissors. At every step, debulking and tumor capsule inspection and dissection from critical surrounding structures was performed before resecting each piece. The extradural clinoidectomy aided in the hemostasis and the resection began at the dural attachment identifying th carotid artery. Secondly, the most posterior and medial components were carefully detached from parasellar cisterns identifying the III nerve and the posterior comunicating artery. Finally, the most anterior and medial components of the tumor compressing the optic nerve were tackled.
Small residue of tumor that was attached to the optical nerve was left, achieving a Simpson grade IV, due to decrease of 50 % on the visual evoked potentials despite irrigation. The tumor specimen was sent to pathology along with the extracted clinoid process. Clear hemostasis was achieved utilizing a combination of bipolar electrocautery and saline irrigation.
The dura was subsequently closed with a running non-absorbable braided 4-0 silk suture. The bone was secured in place utilizing plates and screws. The temporal muscle was reattached to the superior temporal line with 2-0 braided absorbable suture (Polysorb) using small drill holes. Periostium and subcutaneous layer were sutured with simple inverted knots of 2-0 synthetic absorbable suture (Polysorb). The skin was then closed with an intradermal running absorbable suture 3-0 (Monosyn). A small silicon Blake drainage was placed in the subperiosteal space. A sterile head dressing was placed over the closed wound.
Neurophysiological monitoring besides visual evoked potentials remained stable throughout the entire case. All sponge and instrument counts were correct at the end of the case times two. Pupils remained symmetric and with normal size. The patient tolerated the procedure well and was transferred to the recovery room in stable condition.
POSTOPERATIVE EVOLUTION:
The patient awaken with no neurological deficits, spared frontal eyebrow movement, oriented, with normal speech and no weaknesses. Visual accuracy was tested as normal without changes respect to preoperative setting after 3 days, when the swollen eyelid restored to normal. Hence, the intraoperative decrease of visual evoked potentials was considered as a false positive. MRI showed near total resection besides this residue, with no complications. Discharge was given at postoperative day 5 with appointment for follow up.
HISTOLOGICAL DIAGNOSIS:
Meningioma WHO I
NUANCES AND DECISION STRATEGY:
- Check for middle clinoid on CT scan to avoid injury to the carotid artery
- Study MRI T2 sequence to predict consistency of tumor and understand preserved subarachnoid spaces and relationship to neurovascular structures
- Place small hypoallergenic strips on to the ipsilateral eyelid in the prepping, to reduce postoperative swelling
- Perform extradural clinoidectomy to devascularize the tumor early
- Unroof the optic nerve to avoid damage while later manipulating the tumor
- Copious irrigation during drilling to avoid heat damage to the optic nerve
- Preserve internal temporal muscle fascia, avoid cautery on the deep temporal arteries and reattach temporal muscle to the superior temporal line without cutting a cuff to prevent atrophy.
- Avoid bipolar cautery to preserve arachnoid plane as dissection plane, use sharp dissection instead
- High magnification is paramount to detect attachments of small neurovascular structures like anterior coroidal artery or compressed trochlear nerve to the tumor capsule
- Apply ice to reduce orbital inflamation in the postoperative setting