Giant Anterior Falcine Meningioma
Published:
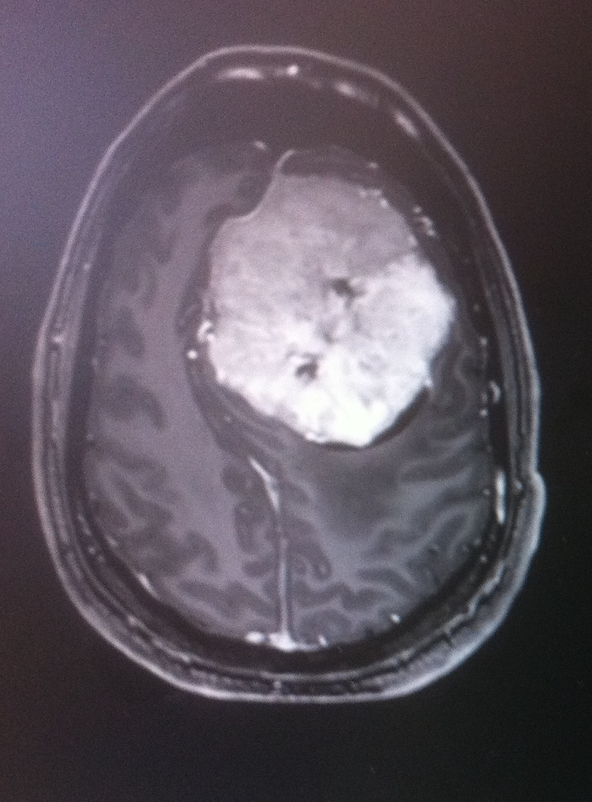
Large anterior falcine contrast enhancing mass
HISTORY:
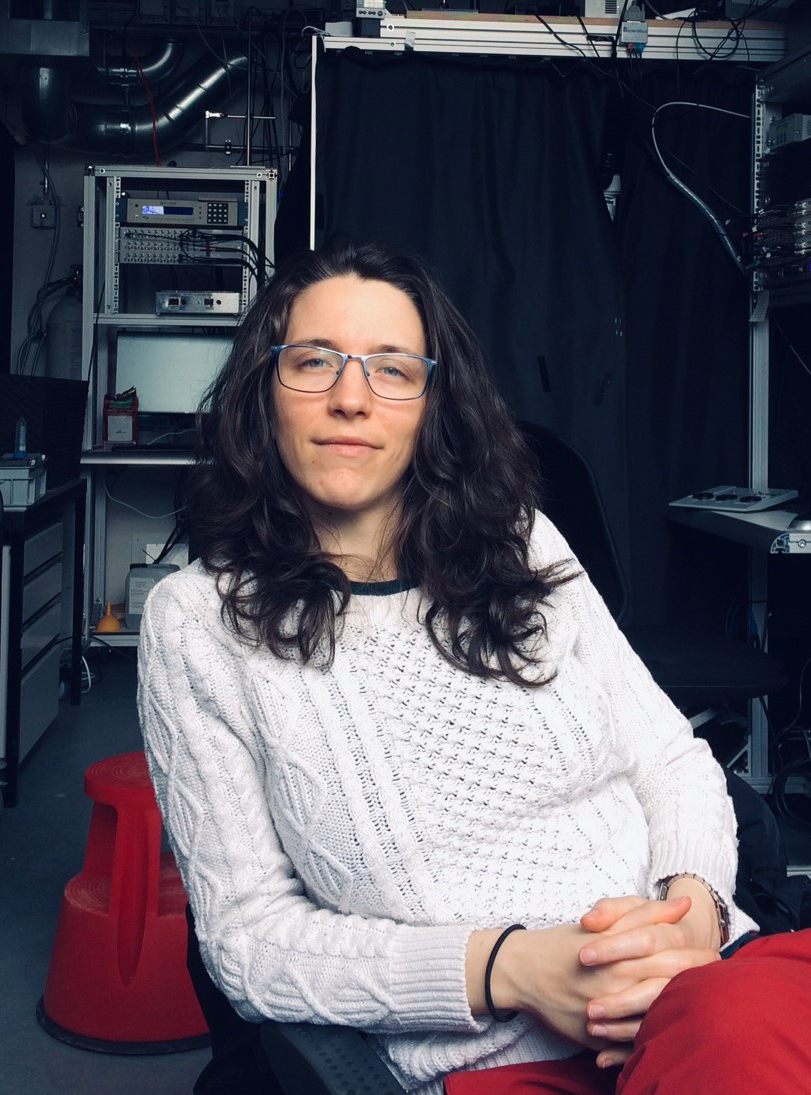
38 year old male who presents with a history of non-controlled headaches. He came to the emergency room suffering a severe headache episode. Radiographic findings were consistent with a large falcine mass. Besides subtle underperformance on daily cognitive tasks, the neurological exam was normal .
DIAGNOSTIC STUDY:
MRI brain showed large anterior falcine contrast enhancing mass, with complete invasion and occlusion of mid-anterior segment of the superior sagittal sinus, compatible with a meningioma with important mass effect and edema.
SURGICAL APPROACH:
Bicoronal Midline extended parasagittal
POSITIONING:
A Mayfield head clamp was applied. The patient was placed in supine position with the head slightly flexed and elevated. Legs were also flexed and kept high, placing the bed axis such that the head stayed slightly below the level of the heart. All pressure points were well-padded. The hair was clipped over the planned incision. Pre-prepping was done with chlorhexidine solution. The electrophysiology monitoring team inserted needles in their proper locations and baseline SSEPs and motor evoked potentials were obtained. The patient underwent co-registration of the preoperative stereotactic MRI with his surface landmarks. The craniotomy was outlined according to the registration to expose healthy duramater margins.
OPERATIVE TECHNIQUE:
The area was prepped and draped in the standard sterile fashion. A bicoronal incision behind the hair line and centered on the lesion, was planned and infiltrated with lidocaine and opened sharply using a #21 scalpel blade. A large periostium flap was dissected separately and preserved for later reconstruction of the duramater. The scalp and the external table of the calvaria bone were noted as normal with no hypertrophic arteries.
A large craniotomy centered over the midline and slighlty posterior to the coronal suture was performed using an electric high speed drill. Two burr-holes were placed at the edges of the craniotomy over the midline and in expected healthy duramater surface. With the help of a #3 Penfield the duramater of the sagittal sinus was disected from the bone and the craniotomy was completed with the craniotome in two passes (from medial to lateral). The bone flap was uplifted utilizing a combination of #3 Penfield and Adson periosteal elevator with special care for the superior sagittal sinus. The dura was noted to have some tears with tumor components strongly adhered to the uplifted bone.
The operating microscope was then draped and brought into the operative field. Initial durotomy was performed bilateraly in a C-fashion with base towards the midline and in healthy duramater. The lesion was noted to be whitish in color with rubbery consistency and clear-defined planes. Using a combination 5-French suction, bipolar electrocautery, as well as micro-scissors a plane was developed around the lesion in both lateral borders at each of both sides of the interhemispheric fissure. The tumor capsule was dissected from the cortical surface and cauterized shrinking and devascularizing the tumor to proceed with a piecemeal resection also using the ultrasonic aspirator for debulking. In the most inferior and deep margin of the tumor, feeding arteries that came from the cingulate and pericallosal arteries were cauterized and cut. The affected falx and venous segment in the superior sagittal sinus were tackled the last, to avoid compromising the venous drainage of the tumor while resecting it.
, To remove the affected falx, origin of the tumor, first, the superior sagittal sinus was temporarly clipped to prove that effective venous outflow was residual. After 10 minutes of unchanged neurophysiology monitoring and no edema development, the affected segment of the sinus was ligated and cut. The falx was then further cut down to the inferior margin and removed "en-bloc", reaching healthy dura, sparing the inferior sagittal sinus that had developed as a collateral pathway and was hypertrophic. Therefore, Simpson grade I was achieved.
The tumor specimen was sent to pathology. The surgical bed was subsequently irrigated until clear hemostasis was achieved utilizing a combination of bipolar electrocautery and oxidized cellulose absorbable hemostat (Surgicel) and liquid hemostat (Surgiflo) .
The large duramater defect was then reconstructed, with a large patch of autologus periostium that had been harvested in the early steps of the surgery, and sutured with a running non-absorbable braided 4-0 silk suture. The internal table of the calvarial bone was drilled down until healthy bone was noted. The bone flap was then secured in place utilizing plates and screws. Subcutaneous layer was sutured with simple inverted knots of 2-0 synthetic absorbable suture (Polysorb). The skin was then closed with an intradermal running absorbable suture 3-0 (Monosyn). A small silicon Blake drainage was placed in the subperiosteal space. A sterile head dressing was placed over the closed wound.
Neurophysiological monitoring remained stable throughout the entire case. All sponge and instrument counts were correct at the end of the case times two. The patient tolerated the procedure well and was transferred to the recovery room in stable condition.
HISTOLOGICAL DIAGNOSIS:
Meningioma WHO II
POSTOPERATIVE EVOLUTION:
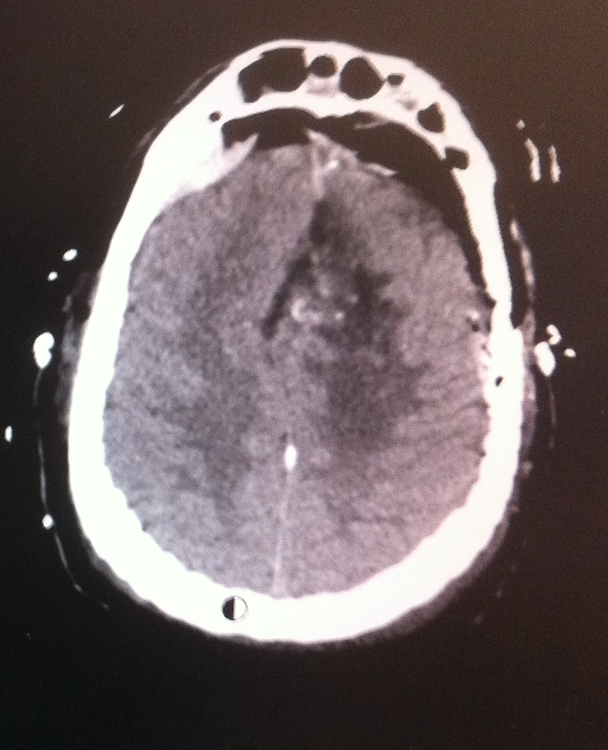
The patient awaken with no complications and with subjective improvement of pressure feeling and headache. Postoperative CT showed gross total resection with no complications. Dexamethasone and Levetiracetam were maintained for several weeks and discontinued slower than in standard cases, due to removal of giant tumor (>60mm in diameter) that produces a drastic change in intracranial pressure and potential exacerbated edema. Discharge was given at postoperative day 7 with appointments for follow up.
NUANCES AND DECISION STRATEGY
- CT bone - study abnormal anatomy of affected bone and venous drainage - diploic veins anatomy and scalp artery
- Prepare blood transfusion and hemostats
- MRI - study vasculature of scalp and duramater that may feed the tumor - prevent important hemorrhage during craniotomy
- Preoperative venous sequence MRI to study the venous system - patency occlusion of venous sinus and developed collaterals pathways
- Avoid sacrifice of patent venous collaterals pathways
- T2 sequence - predicting consistency of tumor and relationship neurovascular structures
- Keep surgical field moist to avoid venous gas embolism and venous sinuses covered with moist cottonoids specially
- Temporal ligation of venous sinus before cutting - wait for 10 min neurophysiology changes and effect on tissue congestion
- Appropriate hidration, corticoid and antiepileptic medication in postoperative setting - drastic change of pressure and decompresion