Dorsal Hemangioblastoma
Published:
Intradural intramedullary contrast enhancing lesion
HISTORY:
52 year old female presents with a history of backpain and increasing paresthesias in both feet. Radiographic findings were consistent with a dorsal intradural intramedullary mass. The neurological exam was normal besides subjective paresthesias in both S1 root dermatomas.No hyposthesias or abnormal bladder or bowel function were noted. Strength was also noted as normal by groups with no walking abnormalities.
DIAGNOSTIC STUDY:
Dorsal MRI showed contrast enhancing mass compatible with a hemangioblastoma...
SURGICAL APPROACH:
Dorsal midline laminoplasty
POSITIONING:
The patient was placed in prone position with t. All pressure points were well-padded. Radiographic control was performed to determine the vertebral bodies at the level of interest to outline the planned incision. Pre-prepping was done with chlorhexidine solution. The electrophysiology monitoring team inserted needles in their proper locations and baseline SSEPs and motor evoked potentials were obtained. Baseline SSEPs showed slight decrease on the right leg.
OPERATIVE TECHNIQUE:
The area was prepped and draped in the standard sterile fashion. A midline incision was done sharply using a #21 scalpel blade. Subcutaneous dissection was performed with monopolar electrocautery reaching the fascial plane. The midline fascia was incised sparing the interspinous ligament, and further proceeded with subperiostic dissection of the laminae. And Adson separator was placed to expose the laminae plane. Plates and screws were plepated for later laminoplasty. With the use of Kerrison #2, small notches at the inferior border of each lamina were done. This helped to perform the lamina cuts with the aid of a craniotome. The three level lamina of levels D5-7 were uplifted en bloc utilizing a #3 Penfield with special care to the duramater. The dura was noted to be intact. Hemostasis of the epidural space was performed with oxidized cellulose hemostat (Surgicel).
The operating microscope was then draped and brought into the operative field. A midline linear durotomy with a #11 scalpel blade using a Milligan dissector in the subdural space guiding the cut. The dura was lifted laterally to both sides with tenting sutures. A caudal electrode was placed in epidural space to record D-wave throughout the case. The tumor was evident from first inspection prtruding into the subarachnoid space. First steps of dissection were focused on identifying involved roots, pial feeding arteries and importantly, the drainage vein of the tumor located at the cranial pole.
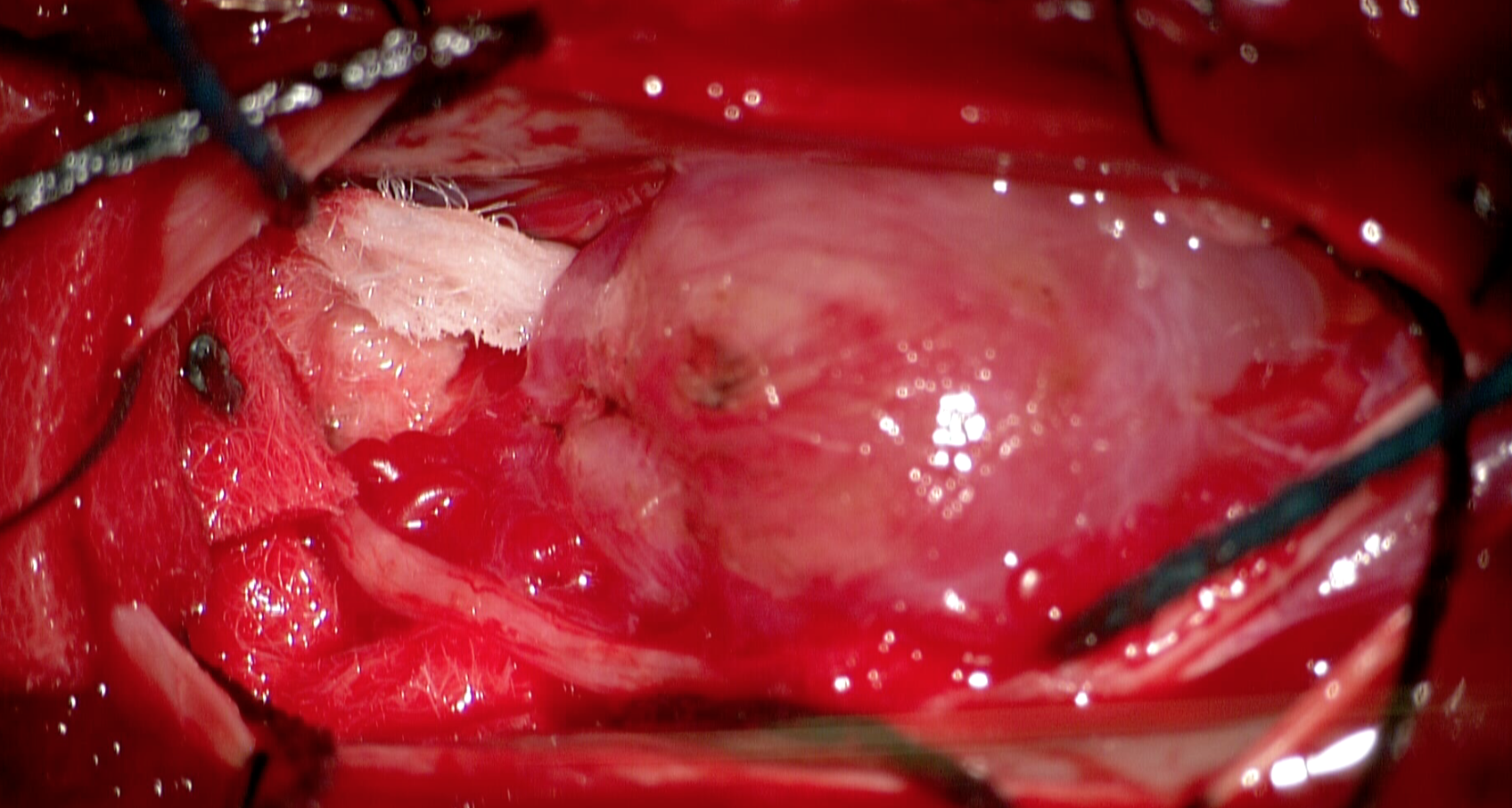
Sharp microdissection with microscissors, bipolar electrocautery and Rhoton dissector #3 was performed to separate attached nerve root to the tumor capsule. The arachnoidal plane was further developed to isolate the main drainage vein. The tumor dissection began at the caudal pole. With a combination of bipolar electrocautery, suction and microscissors, the surface of the tumor was coagulated and devascularized while dissecting it from the pial plane. The lesion was noted to be reddish in color with rubbery consistency and clear-defined planes. The plane was completed around the lesion coagulating pial arteries and sparing the drainage vein at the cranial pole. Piecemeal resection was avoided and removal was made en bloc after coagulating the drainage vein as the last step.
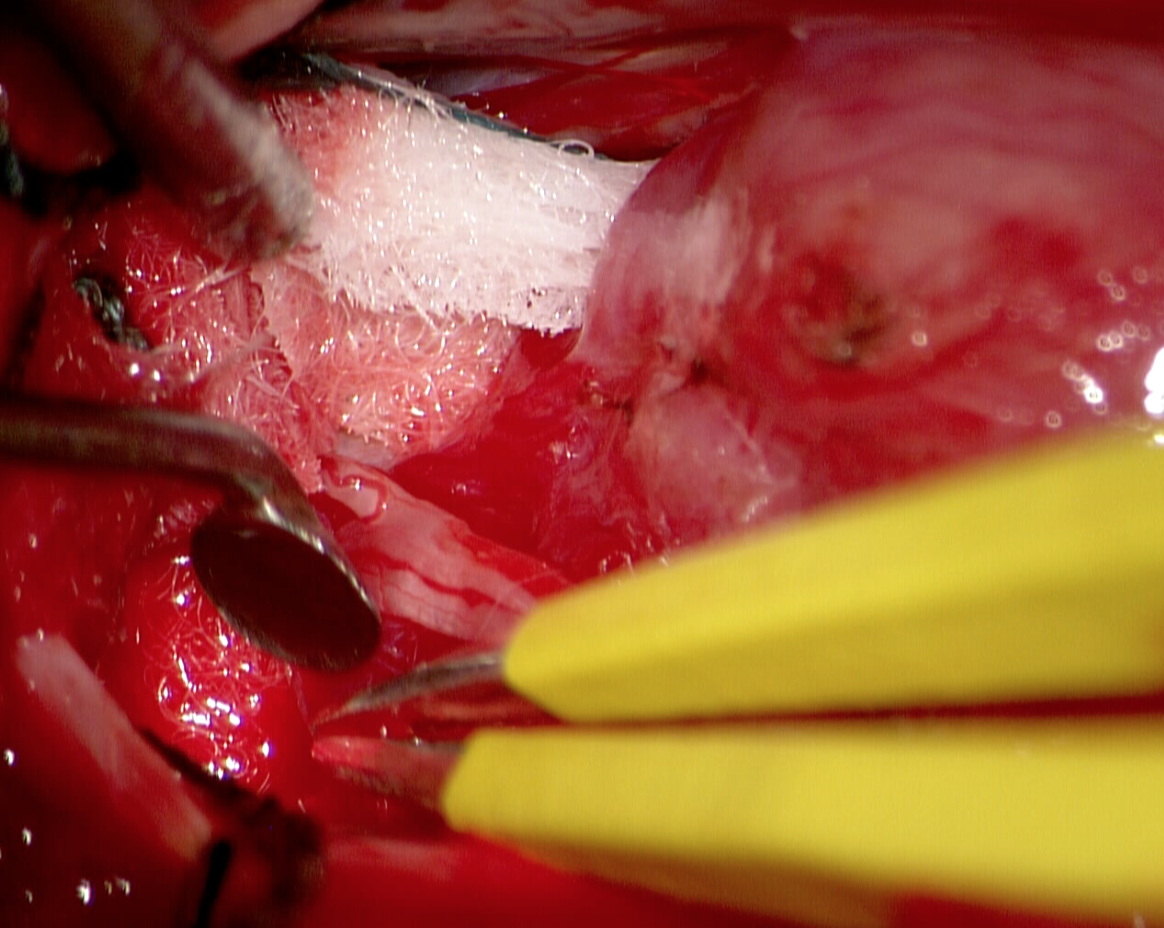
The tumor specimen was sent to pathology. The surgical bed was gently irrigated until clear hemostasis was achieved with no electrocautery.The dura was subsequently closed with running non-absorbable braided 4-0 silk suture ensuring a water tight closure. The laminae were replaced and secured in place at each level utilizing plates and screws. Muscle was approximated to the midline and anchored to the spinous process. The fascial plane was reattached to interspinous ligament that was resutured both proximally and distally. Subcutaneous layer was sutured with simple inverted knots of 2-0 synthetic absorbable suture (Polysorb). The skin was then closed with an intradermal running 3-0 absorbable suture (Monosyn).
Neurophysiological monitoring remained stable throughout the entire case. All sponge and instrument counts were correct at the end of the case times two. The patient tolerated the procedure well and was transferred to the recovery room in stable condition.
POSTOPERATIVE EVOLUTION:
The patient awaken without new neurological deficits. Postoperative MRI showed gross total resection with no complications. Paresthesias persisted throughout the immediate postoperative period and slowly diminished in intensity. Discharge was given at postoperative day 5 with appointments for follow up and neurophysiology re-evaluation.
NUANCES AND DECISION STRATEGY
- On the opening dissection, preserve interspinous ligament and reattach the fascial plane to it in the closure
- Perform laminoplasty whenever possible
- Intraoperative monitoring D-wave has a high predictive value
- Surgical strategy for resection of hemangioblastomas should be as for vascular malformations: identify feeding arteries and coagulate them, and leave the drainage vein for the end.
- Do not attempt to debulk or do piecemeal resection unless strictly needed and after extensive devascularization since the bleeding is prominent.
- Leave no drainage