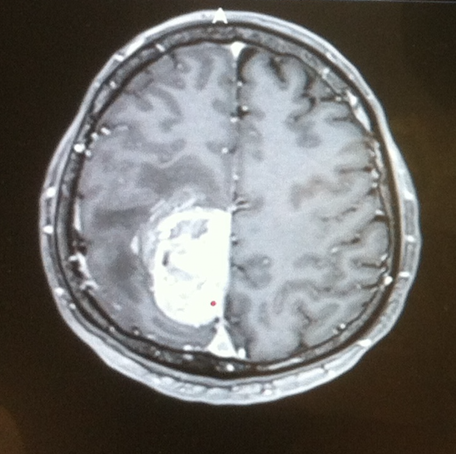
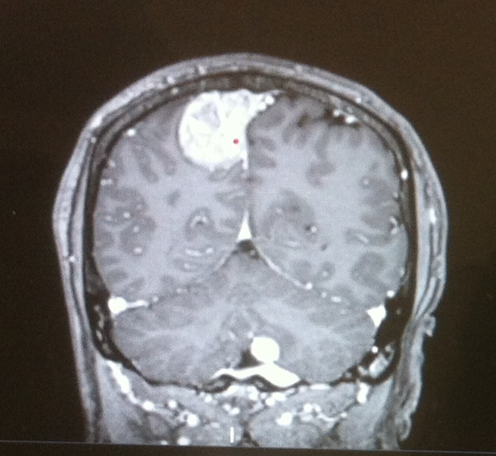
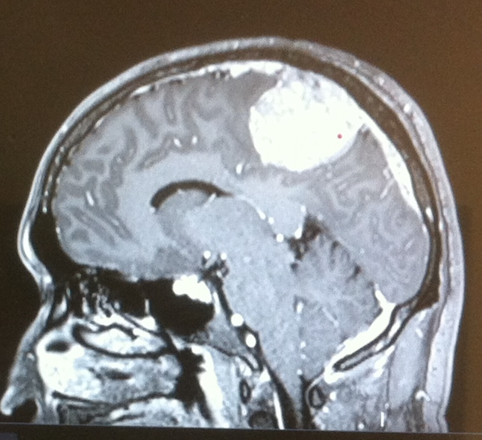
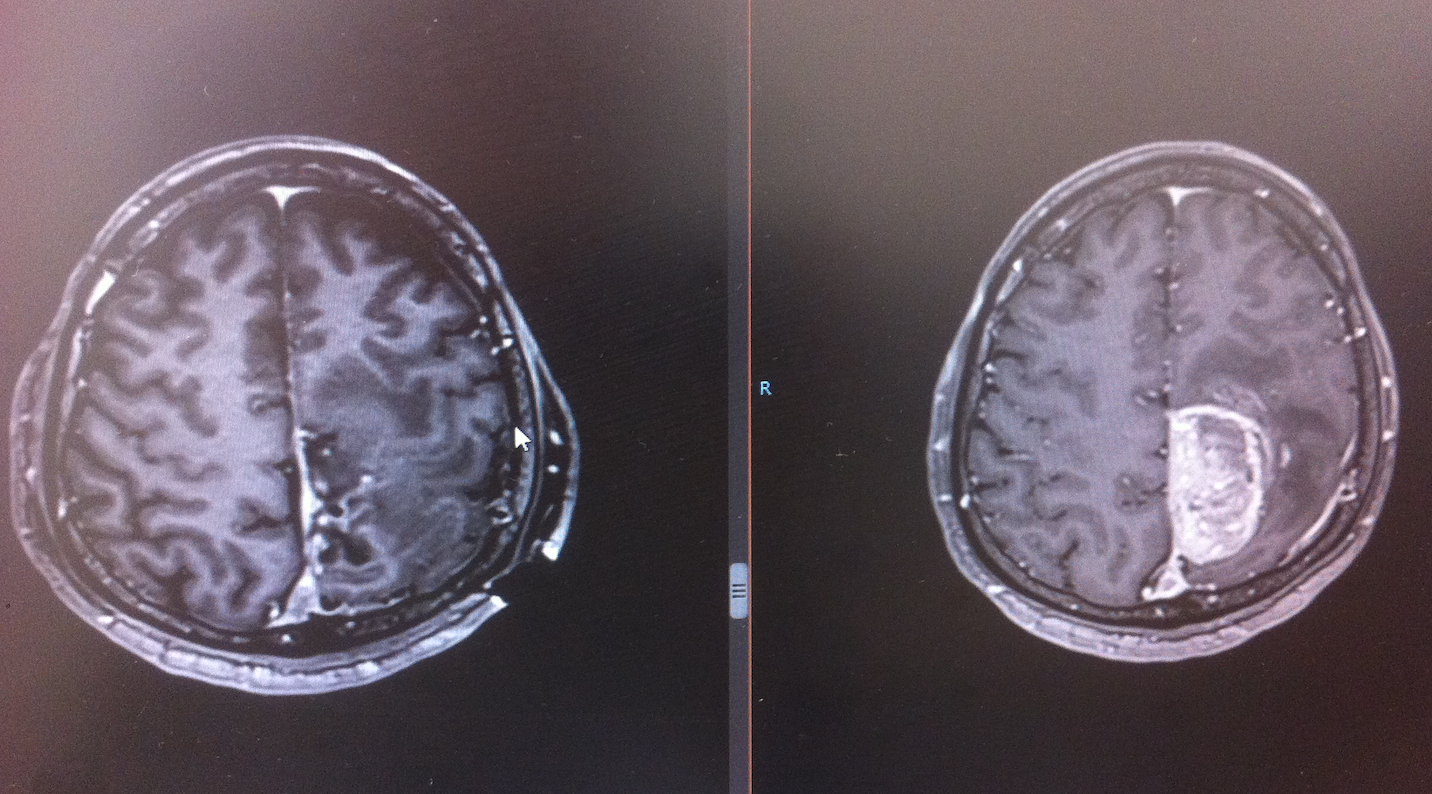
Right Posterior Parietal Meningioma
Published:
Right posterior parietal hemorhagic contrast enhancing mass
HISTORY:
46 year old male who is brought to the emergency room presenting a sudden weakness of the left leg. The neurological exam showed a left leg paresis that precluded stand up position and walking. By segments, strength was 2/5 in all proximal groups and 1/5 in distal ones. Hypoesthesia was also present distally. The rest of the examination appeared normal.
DIAGNOSTIC STUDY:
MRI brain showed right parietal parasagittal extra-axial contrast enhancing mass with a recent hemorrhage compatible with a meningioma. The MRI further demonstrated that the superior sagittal sinus was patent but partially invaded. Additionally, the meningioma continued along the sagittal sinus following the transverse sinus and the sigmoid sinus, to the posterior fossa, where another small meningioma mass was present with no surrounding edema or compression.
SURGICAL APPROACH:
Posterior parasagittal
POSITIONING:
A Mayfield head clamp was applied. The patient was placed in supine position with the head and trunk slightly flexed and elevated but keeping them at heart level. All pressure points were well-padded. The hair was clipped over the planned incision. Pre-prepping was done with chlorhexidine solution. The electrophysiology monitoring team inserted needles in their proper locations and baseline SSEPs and motor evoked potentials were obtained. The patient underwent co-registration of the preoperative stereotactic MRI with his surface landmarks.
OPERATIVE TECHNIQUE:
The area was prepped and draped in the standard sterile fashion. A linear parietal incision, parallel to the coronal suture, was planned and infiltrated with lidocaine and opened sharply using a #21 scalpel blade. Periostium was disected separately and preserved in case of dura reconstruction.
Right parietal parasagittal craniotomy was performed using an electric high speed drill. Four small burr-holes were placed at the corners of the craniotomy, dissecting the dura over the sinus from the skull.The bone flap was uplifted utilizing a combination of #3 Penfield and Adson periosteal elevator with special care for the midline sagittal sinus. The dura was noted to be intact. The bone dust was irrigated and suctioned clean. A small C-shaped durotomy with base towards the midline was performed and the dura was lifted with tenting sutures, keeping the dura over the sinus moist and without tension.
The operating microscope was then draped and brought into the operative field. The tumor was immediately in sight with two large cortical bridging veins on its surface that drained to the sagittal sinus. The lesion was noted to be gray-redish in color with rubbery consistency and well-defined planes. It was also congested and prompted to bleed with any attempt to manipulate it. Careful dissection of the interhemispheric fissure was carried out to identify clear tumor margins and dissect them from the cortical surface. Cottonoid patties were placed on the cortical surface to avoid injury during dissection and were kept moist throughout the procedure. The attached cortical bridging veins were dissected from the superior tumor capsule and preserved. Microdissection technique was further used to slowly devascularize the tumor and debulk it in a piecemeal fashion. A small intratumoral hemorrhage was noted and suctioned, matching the radiological findings. Continous hemostasis with bipolar electrocautery, oxidized cellulose absorbable hemostat (Surgicel) and liquid hemostat (Surgiflo) was necessary due to the high venous congestion of the tumor. Since the sagittal venous sinus was partially invaded and the meningioma spread all along it up to the posterior fossa, the resection was limited to the parietal mass (Simpson grade IV). The dural attachment of the tumor to the sinus was cauterized.
The tumor specimen was sent to pathology.The surgical bed was subsequently irrigated until clear hemostasis was achieved. Cortical bridging veins remained intact and with proper flow.
The parietal dura, which appeared healthy and separated from the original tumor, was subsequently closed with running non-absorbable braided 4-0 silk suture. The bone was secured in place utilizing plates and screws. Periostium and subcutaneous layer were sutured in separate plantes and with simple inverted knots of 2-0 synthetic absorbable suture (Polysorb). The skin was then closed with an intradermal running absorbable suture 3-0 (Monosyn). A small silicon Blake drainage was placed in the subperiosteal space. A sterile head dressing was placed over the closed wound.
Neurophysiological monitoring showed improvement in MEPs of the left leg respect to the baseline obtained at the beginning of surgery. All sponge and instrument counts were correct at the end of the case times two. The patient tolerated the procedure well and was transferred to the recovery room in stable condition.
HISTOLOGICAL DIAGNOSIS:
Meningioma WHO I
POSTOPERATIVE EVOLUTION:
The patient awaken without new neurological deficits and with subjective improvement of the strength in the left leg. Over the postoperative days, the patient started to gain strength and initiated walking with the help of a walker. Proximal weakness improved greatly allowing him to stand autonomously. However, distal strength improved more slowly and the left foot drop interfered greatly in his walk pattern. Postoperative MRI showed gross total resection of the mass with no complications, with persistent disease along the venous system and posterior fossa. Antithrombotic therapy was introduced following guidelines as in standard cases, but maintained for a longer period to avoid thrombosis of manipulated veins and partially occluded sagittal sinus. Discharge was given at postoperative day 5 with appointments for follow up and rehabilitation protocol.
NUANCES AND DECISION STRATEGY
- Study preoperative venous MRI - study venous system anatomy and check patency of infiltrated venous sinsuses
- Do not attempt Simpson grade I with patent sinus if reconstruction of sinus venous flow is not possible
- Ressection of a venous sinus segment without reconstruction is only tolerated in completely occluded sinuses or very anterior segments of superior sagittal sinus.
- Do not sacrifice cortical bridging veins – parietal are thick - mortality postoperative edema
- Study anatomy of venous collateral pathways that developed because of the tumor, and preserve them
- Parietal region is very rich in venous drainage so interruption or sacrifice of venous flow can lead to venous congestion, hemorrhage and venous infarction - Postoperative mortality rate is still high, as compared to other procedures and locations, and related to raised intracranial pressure due to secondary edema after interruption of venous flow due to surgical strategy or postoperative thrombosis
- Be prepared and prevent air embolism keeping venous sinuses covered with moist cottonoids at all times. Constantly monitor with the anesthesiology team and in case of an event use Trendelemburg positioning lowering the surgical field height below the heart level to increase venous pressure and irrigate copiously.
- Accessible central venous line to absorb air bubbles is mandatory